Making hormone health support safe, normal and accessible at work
For many employees, hormone health is something they manage quietly, privately and often in isolation. Not because it isn’t affecting their work — but because talking about it can feel unsafe. Too personal. Too exposing. Too embarrassing. Or worse, that it will lead to them being labelled as “hormonal”, unreliable or not quite coping.
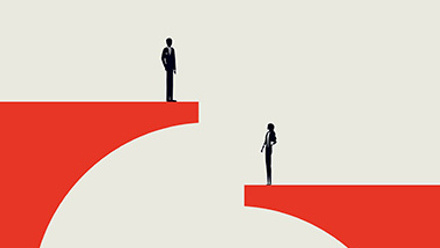
Despite years of progress on workplace wellbeing, hormone health remains one of the last taboos at work. It affects millions of employees every day yet is still rarely discussed openly - and even less often supported by employers.
According to research by the NHS Confederation, an estimated £11bn is lost every year due to absenteeism linked to gynaecological conditions such as heavy and painful periods, endometriosis, fibroids and ovarian cysts.
Separate research shows almost a quarter (23%) of working women have considered quitting due to the impact of menopause or menstrual symptoms at work, and 87% of working women want their employer to be more supportive when it comes to women’s health.
Recent CIPD research shows that 57% of women experiencing menopause say it has negatively affected their career progression. Symptoms such as fatigue, brain fog, anxiety and disrupted sleep are common - and directly affect performance, confidence and retention.
Why hormone health support is failing working women
A renewed focus on women’s health at a national level suggests momentum is finally building.
In October last year, the government announced that the Women’s Health Strategy will be refreshed as part of its 10 Year Health Plan, with a stated commitment to listening to women’s experiences and addressing inequalities across gynaecological health, menstrual health and menopause. It has, however, yet to translate into consistent, practical change in everyday working life.
Meanwhile, in many workplaces, hormone health support remains fragmented. Fertility benefits sit in one corner of the benefits strategy, menopause policies in another, with little recognition of the broader hormonal journey employees navigate across decades of working life.
For savvy people-focused organisations, the renewed national focus on women’s health should act as a prompt to rethink this approach. For many women, this gap is not theoretical.
Midlife is often where fertility concerns, hormonal changes and career pressure collide - yet workplace support is still largely framed as either “fertility” or “menopause”, with little in between. Uncertainty about symptoms, limited guidance and the sense that you are navigating it alone can leave employees quietly researching, self-managing and second-guessing what is happening to their bodies.
Even where workplace benefits exist, the more pressing question is often not whether support is available, but whether it feels safe, confidential and normal enough to use.
Creating a culture where support feels safe to use
For HR and reward leaders, the challenge is about creating an environment where using benefits feel psychologically safe.
That means:
- Normalising conversations about hormone health
- Making support inclusive for all genders and age groups
- Promoting benefits proactively
- Emphasising confidentiality and choice
- Training managers to respond with empathy
When hormone health support is positioned as preventative, routine and available to everyone it becomes far more accessible.
How to offer safe, normal and accessible support
- Normalise hormone health as part of everyday wellbeing: Position hormone health alongside mental health, sleep and musculoskeletal support — not as a specialist or “women-only” issue. Regular, neutral communication helps remove the sense that accessing support is exceptional or risky.
- Focus on early insight, not just crisis support: Many employees don’t know whether what they’re experiencing is hormonal, stress-related or something else. Providing access to preventative health screening and guidance helps employees understand what’s happening earlier - before symptoms escalate or performance suffers.
- Design for discretion and choice: Even in supportive cultures, not everyone wants to raise personal health issues with a manager or HR. Benefits that can be accessed confidentially and independently are more likely to be used - particularly for sensitive issues such as fertility, menstrual health and menopause.
- Make inclusivity explicit: Hormone health affects people of all genders and ages, yet is often framed narrowly. Being clear that support is inclusive - and relevant beyond a single life stage - helps reduce stigma and encourages wider engagement.
- Equip managers to respond, not diagnose: Managers need the confidence to listen without judgement and signpost support appropriately. Empathy, flexibility and avoiding assumptions matter more than medical knowledge.
- Promote consistently, not just once: Regular reminders, clear signposting and leadership endorsement help embed hormone health support as a normal part of working life.
Why this matters now
Employees don’t leave parts of their biology at the door when they come to work. Hormonal health shapes how people think, feel and perform — often invisibly.
The companies that will make the greatest impact are not those offering the longest list of benefits, but those creating cultures where using them feels safe, routine and judgement-free. When hormone health becomes part of normal working life, employees no longer have to choose between protecting their health and protecting their careers.
Supplied by REBA Associate Member, Avantus
Flexible Benefits & Technology specialist providing online, highly configurable platforms to Customers and Intermediaries worldwide.