Hormone imbalance and mental health: why every wellbeing strategy needs to understand this link
Hormones – like most things in life – need to be kept in balance. There are periods for both men and women where hormone fluctuations are inevitable and sadly, they can have a severe impact mental health.
The link between hormone health and mental health is well known in medical circles, but it’s not something widely discussed in a workplace context.
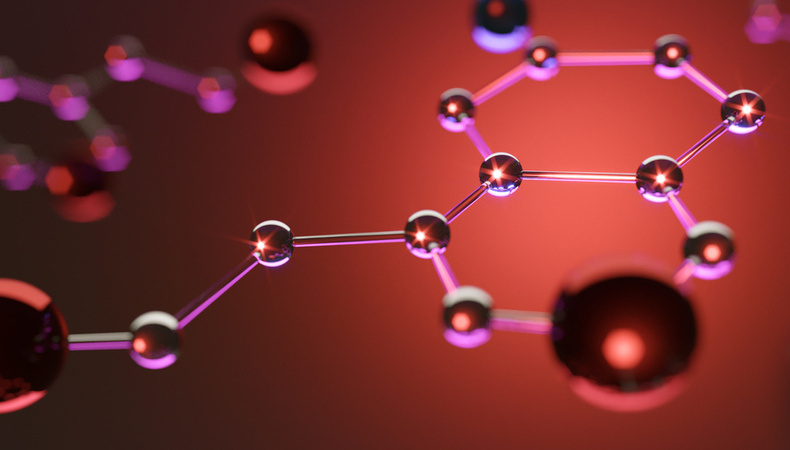
Decoding the science
There are three main sex hormones: oestrogen, progesterone and testosterone. Another hormone associated with this group is oxytocin. This is in turn linked to serotonin, and each enhances the other’s production. Oxytocin and serotonin are our “happy hormones”. When these levels are low, people are unable to feel any joy; instead they may feel anxious or depressed.
The main sex hormone for women is oestrogen. Oestrogen has many wonderful qualities; it helps to maintain bone strength and boosts the health of skin, hair, nails – and, crucially, mood. It is also a key regulator of serotonin. During periods where oestrogen levels become erratic or depleted – such as during perimenopause or menopause or just before a period starts – this can lead to a number of implications such as loss of motivation, depression, impaired cognitive function, anxiety and mood swings.
Similarly, progesterone is a calming hormone which aids sleep and cognitive function. When this hormone is dysregulated, women are likely to experience sleep issues, anxiety, irritability, depression and stress.
Imbalances
The emotional strain of hormonal imbalance is more common among women, as they experience more severe fluctuations during menstruation, childbirth and post-natal, and peri-to-post menopause. For women with existing mental health issues, these fluctuations can exacerbate their suffering. For example, studies revealed that 64% of women with major depression said their symptoms got worse five to ten days before their period starts.
Testosterone is usually thought of as the male hormone. Women also produce it; however, they require much smaller quantities than men. Testosterone is also integral to wellbeing. It is great for confidence, lowers stress and generally provides people with a much more positive sense of wellbeing. As with all hormones, it has a direct effect on mental health when the balance is impaired. Symptoms for both excessively high and low levels of testosterone include increased anxiety, indecisiveness, irritability, aggressiveness insomnia, low confidence and memory loss.
One million British men are estimated to have testosterone deficiency, but symptoms like fatigue are often passed off as signs of ageing and currently, only 8% of potential patients get treatment. Those at highest risk are men over 50, or those who have a high BMI. Taking certain medications can also lead to low testosterone.
Why is any of this a workplace issue?
This is something we hear quite often. Are these conditions not covered by private medical insurance? Are hormones not a deeply personal matter?
There are several points to note here. Firstly, private medical insurance cover does vary enormously. Some policies do cover hormone-related conditions, such as fertility and menopause. However, many do not – and even those which do may only offer a limited service. What’s more, people don’t always recognise what might be happening to them.
There have been an increasing number of stories coming to light of women being misdiagnosed with depression and even early onset dementia, when they were entering perimenopause. Men with low testosterone just thinking they’re “getting old”. Therefore, the more employers can be aware of the signs and help signpost anyone in need, the better.
Yes, hormone health is a personal matter, but only in the sense that it comes with a perceived stigma. Many people don’t feel comfortable talking about it for fear of judgement. For example, one respondent in our recent menopause workplace survey said she believed her career prospects would stall; that she would be viewed as “past her sell by date”.
Increasing awareness
It seems likely, with all the recent media coverage around the menopause, menstrual health and fertility, that the tide is turning.
However, workplaces should still be mindful of hormonal changes and ensure they create safe spaces for employees to talk about their challenges, if they choose to. Line managers should be trained to be aware of the signs that someone may be struggling with their hormones, as a key component of mental health training.
The link between hormone health and mental health is clear. The knock-on effect for employers could be decreased motivation, job satisfaction and engagement. However, those businesses which equip themselves with knowledge of hormonal health, compassion and a culture of openness will be rewarded with a happier, healthier and far more productive workforce.
This article is provided by Fertifa.
Supplied by REBA Associate Member, Fertifa
Leading health benefits provider, offering best-in-class clinical care for neurodiversity and reproductive health.