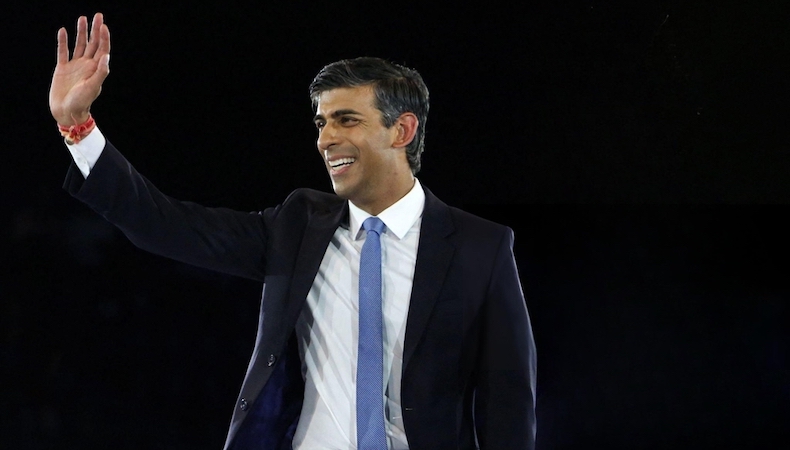
Why Rishi Sunak’s plan to end sick-note culture is doomed to fail
Last month, Prime Minister Rishi Sunak announced plans to tackle what he calls “sick-note culture”.
In a video posted on his Facebook page, he explained the rationale behind the changes: “There’s been a massive rise in people of working age who are inactive and unable to work because of ill health or sickness conditions.”
He outlines the scale of the problem:
- The number of people identified as not being able to work by the Work Capability Assessment (WCA) has tripled since 2011
- Annual welfare spending for disability and sickness conditions has risen 63% since the Covid-19 pandemic (currently £69bn – more than schools, policing or transport)
- Personal independence payments (a disability benefit known as PIP) are forecast to rise by 50% over the next four years.
Few would argue with the prime minister’s statement that something isn’t working.
The five-point plan he lays out includes reassigning sick notes to other professionals to relieve pressure on GPs – a change mostly welcomed by doctors. It also includes reforms to the WCA, PIP and a crackdown on welfare fraud.
But there was a glaring omission on Mr Sunak’s flip chart, namely anything to do with the healthcare system itself and the unprecedented delays and professional shortages it’s experienced since the pandemic.
Five facts about sickness and sick-note culture
- Currently, 2.8 million people in the UK are limited in their ability to participate in work due to ill health
- The UK loses around 185 million working days to ill-health every year, at an annual cost of £150bn
- Sick notes are officially called, ‘fitness to work notes’ or ‘fit notes’, and certify that an individual has a valid reason for staying off work longer than seven days
- Since 2022, healthcare professionals including nurses, occupational therapists, pharmacists and physiotherapists have been able to issue fit notes, as well as GPs
- NHS data shows almost 11m fit notes were issued last year in England, with 94% of those signed ‘not fit for work’.
Is the UK we really getting sicker?
When examining the tripled rate of those deemed unable to work by the WCA, the prime minister says: “I don’t think people are three times sicker than a decade ago.”
But is he right?
Between 2014 and 2015 just over 2.9m people in the UK had diabetes. Diabetes.uk now estimates this figure to be 5 million (just under twice as many).
Meanwhile, around one in four people in the UK today will experience a mental health problem each year – up from one in six in 2014 (one-and-a-half times as many).
And in 2015, Macmillan estimated that 890,000 people were living with cancer; this number now stands at 3 million.
So, when it comes to cancer, people are in fact more than three times sicker than a decade ago. Cancer rates are skyrocketing, and most rapidly among the exact population the prime minister is targeting.
In fact, close to half of all people living with cancer in the UK are of working age.
What cancer can teach us about healthcare and welfare challenges
While the prevalence of cancer is growing (at an alarming rate), death rates from the disease are falling (by 33% since 1991 and continuing to decline by around 1.5% each year).
This means there is a large and growing survivorship population. This should be good news for the government and employers alike, yet it isn’t.
Those living with and beyond cancer can expect to experience a range of side-effects, both from the disease itself and from its treatment.
These challenges can be physical, psychological and practical and, if not supported, have the power to shift someone out of the workforce and into the welfare system (cancer is categorised as a disability from the point of diagnosis).
- Around 85% of people with cancer who were employed when diagnosed say it was important for them to continue to work, yet 57% lack the support they need to do so
- Consider that 40% of prostate cancer survivors experience urinary leakage, and 19% of colorectal cancer patients report difficulty controlling their bowels.
Both of these side-effects can easily prevent people from working, yet both can be supported by specialist cancer physiotherapists.
However, the waiting time to begin musculoskeletal physiotherapy is currently 18 weeks in one NHS trust. That’s a long – and, for employers, costly – amount of time, especially when taken alongside time off for treatment and dealing with other side-effects.
There are even greater barriers to access for cancer-specific physiotherapy, including a shortage of trained professionals.
While physiotherapy is an isolated example of a specialism that many patients may find themselves waiting a long time to access (keeping them off work), delays are universal across the NHS.
The British Medical Association recorded an 87% increase in unsuccessful GP referrals to secondary care between 2019 and 2021, adding: “The care for these patients does not disappear. Instead, these patients need to be cared for by GPs … adding to the pressure in primary care.”
And if overstretched GPs cannot provide that care, that person is certified ‘not fit for work’.
The prime minister’s plans to relieve the pressure on GPs by assigning fit notes to other professionals is unlikely to achieve the desired outcomes unless positioned alongside a robust healthcare strategy that targets the barriers to accessing specialists that prevent people from returning to work.
What innovations in cancer care tell us
The BBC reported that Dr Katie Bramall-Stainer, chairwoman of the BMA’s GP committee, said the prime minister should focus on what is stopping patients from receiving the healthcare they need, which in turn prevented them working.
Clearing the NHS backlog and opening up availability to care at primary and secondary level is much needed but will take years. In the meantime, new ways to get healthcare must be created to support those with chronic conditions to return to and stay in work are urgently needed and already available.
One area that could provide solutions which has been relatively untapped is technology.
Innovations in digital healthcare and AI can provide the expertise and availability the NHS currently cannot.
For example, the average waiting time for a virtual appointment with a cancer-specialist physiotherapist (or a psychologist or dietitian) on Perci Health is 48 hours, and dedicated vocational rehabilitation (with a current 86% success rate) is offered.
When the prime minister says that we need to make changes, he was entirely right, yet the problem is so much more complex than his flip chart suggested. The good news is that innovative solutions already exist – if only Mr Sunak could see them.
Supplied by REBA Associate Member, Perci Health
Perci Health is the first digital platform bridging the gap between cancer and wellness.